Summary:
Climate change could significantly disrupt the global blood supply, putting critical medical treatments at risk, according to a new study published in The Lancet Planetary Health. Researchers from the University of the Sunshine Coast and Australian Red Cross Lifeblood warn that extreme weather, shifts in infectious diseases, and rising temperatures could impact every stage of the blood supply chain – from donor health to storage and transportation.
Dr. Elvina Viennet, UniSC Adjunct Research Fellow, highlighted how natural disasters like floods and cyclones not only limit people’s mobility but also compromise the safety and availability of blood products, which already have a short shelf life. Lead researcher Associate Professor Helen Faddy noted that this is the first study to systematically examine global climate threats across all blood supply stages.
The team found that climate change may also drive the spread of mosquito-borne illnesses such as dengue fever and malaria, restricting donor eligibility and raising demand for blood transfusions. In addition to physical impacts, the study points to psychological effects like climate anxiety potentially influencing donor participation. The researchers call for early warning systems, flexible donor policies, and innovative solutions like drone transport to future-proof blood supplies against an evolving climate.
New study predicts how climate change will jeopardise global blood supply
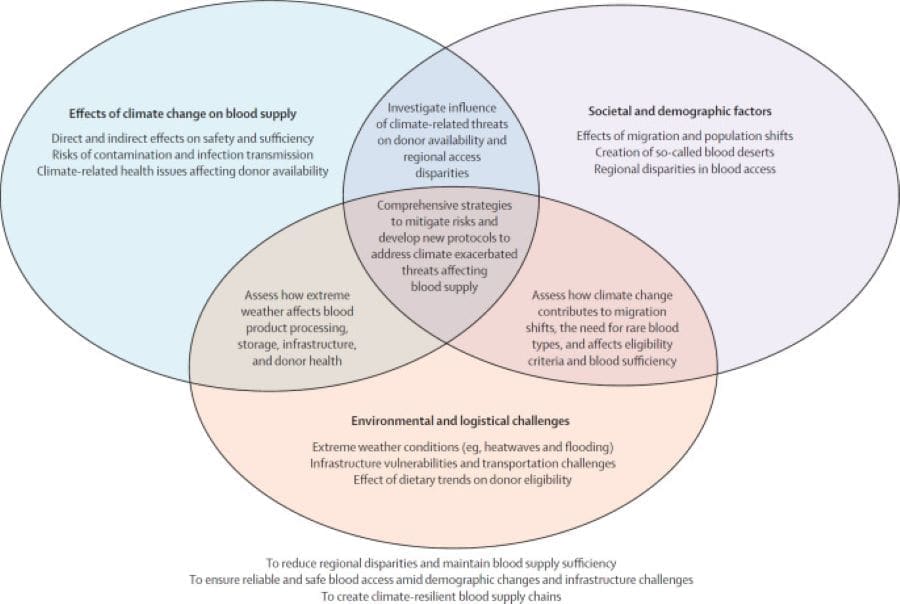
Researchers at the University of the Sunshine Coast and Australian Red Cross Lifeblood say health issues, the spread of infectious disease and extreme weather exacerbated by climate change will impact the ability of people to donate, and at the same time may trigger a rise in the need for blood.

Lifeblood researcher and UniSC Adjunct Research Fellow Dr Elvina Viennet said this threatened the safety and supply of life-saving blood products crucial for surgeries, trauma care, chronic disease management – and saving lives in emergency situations.
“Warmer temperatures and natural disasters such as heatwaves, floods, cyclones and bushfires are expected to become more frequent and severe,” Dr Viennet said.
“As well as limiting the mobility of large numbers of people, these events disrupt the storage, safety, and transportation of blood which has a short shelf life.
“We experienced this recently with ex-Tropical Cyclone Alfred in Australia, when an extreme weather event drastically reduced national blood supplies for the first time.”
Lead researcher, UniSC Associate Professor Helen Faddy said the study was the first to globally examine how a changing climate could affect each stage of the blood supply chain, based on a comprehensive literature review of international studies.
“While many studies have explored the broader health effects of climate change, we sought to fill gaps in understanding the full extent of the risks – from donor health and collection logistics to the processing, storage and distribution of products,” she said.
The finding suggest climate change may impact some infectious diseases that can be transmitted via blood and can prevent people from donating.
“For example, predictions of increased rainfall and warmer temperatures in certain regions including Australia, could intensify mosquito-borne diseases such as Dengue Fever, West Nile Virus and Malaria, and potentially see them spread to new areas,” Dr Faddy said.

“At the same time, shifts in disease prevalence and natural disaster frequency could increase the demand for blood transfusions due to conditions such as pregnancy complications, cardiovascular disease and sickle cell disease.
“We could also face greater difficulty in finding the right blood for patients. With rising sea levels increasing migration rates, it’s essential to have more donors from a variety of ethnic backgrounds, and to increase the number of people who give blood.”
Less obvious health conditions and heat-related illness could also impact donors, staff, and volunteers.
“We could see new diseases emerge, health issues such as blood pressure and hydration that are exacerbated by heat, as well as psychological distress and ‘climate anxiety’, impact donors,” she said.
The study emphasises the need to reduce reliance on traditional blood supply chains and have adaptable strategies that offer rapid responses to climate-related challenges.
The researchers recommend Governments and blood services can prepare with critical tools such as early warning systems, disease surveillance, flexible approaches to donor eligibility and blood transport in emergencies, hospital preparation, and expanding collection services so donations can be relocated quickly.
“Recent global innovations include cell salvage techniques during surgery, the use of drones to transport blood when other transit is disrupted, and walking blood banks, which collect donations at the site of crises,” Dr Faddy said.
“As our environment evolves, we need to reduce reliance on traditional blood supply chains and have adaptable strategies that offer rapid responses to climate-related challenges.”
Journal Reference:
Viennet, Elvina et al., ‘Blood under pressure: how climate change threatens blood safety and supply chains’, The Lancet Planetary Health 9, 4 (2025). DOI: 10.1016/S2542-5196(25)00051-8. Also available on ScienceDirect.
Article Source:
Press Release/Material by Australian Red Cross Lifeblood
Featured image credit: Vince | Pixabay