Incorporating humidity improves estimations of climate impacts on health.
As climate change continues to impact global health, accurate models are essential for governments, medical institutions, and other organizations to effectively plan and respond to health-related challenges.
Traditionally, models assessing the health impacts of climate change have focused primarily on temperature, often overlooking the significant role that humidity plays in exacerbating heat stress.
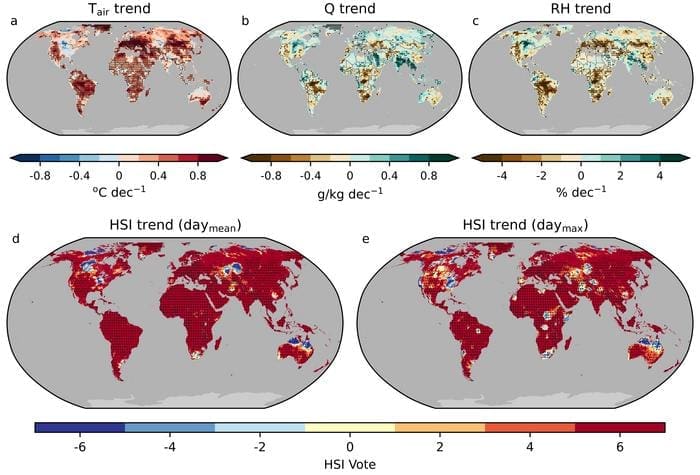
Now, in a new study, researchers from the University of Tokyo have successfully integrated humidity data into heat stress indicators (HSIs), improving the accuracy of predictions related to heat-related mortality.
Climate change, referred to as global warming for a good reason, is recognized for driving temperature increases worldwide. However, the impact of climate change extends beyond just rising temperatures. Humidity – the concentration of water vapor in the air – is a critical factor in how the human body perceives heat.
High humidity levels can impair the body’s natural cooling mechanism through sweating, as evaporative cooling becomes less effective. This can lead to dangerous levels of heat stress, particularly in regions where humidity is high.
“I’d been investigating the effect of irrigation around urban areas on heat stress, and how it is related to human health,” explained Qiang Guo, a research fellow from the University of Tokyo’s Department of Global Health Policy. “Depending on what HSIs you looked at, the results and implications appeared quite different. This discrepancy pushed my team and me to look for the best combination of temperature and humidity which would most accurately estimate human-perceived heat stress. And we wanted to make sure this method would apply to different environments.”
To address this gap, Guo and his team gathered comprehensive climate and mortality data, including air temperature, relative humidity, wind speed, and incident solar radiation, from 739 cities across 43 countries and territories. They calculated eight different HSIs using this climate data. While most HSIs typically incorporate air temperature and humidity, others also include factors like wind speed and solar radiation.
By utilizing advanced models, including distributed lag nonlinear models and machine learning, the researchers identified the crucial role of the relationship between daily temperature and humidity in determining the effectiveness of HSIs.
“The effectiveness of HSIs incorporating humidity varies according to geography. We detected locations where humid heat is a more accurate predictor to model heat-related deaths, including coastal and large lake areas of the U.S., Peru, South Korea, and Japan. Utilizing HSIs in these regions, such as wet bulb globe temperature, which mimics how humans feel heat, could improve accuracy of heat-health alert systems,” said Guo.
The study also acknowledged limitations.
Due to data availability, the research primarily focused on developed regions, leaving many developing regions – where heat stress can be severe – underrepresented. Recognizing this, Guo emphasized the importance of expanding future studies to include these regions. “Our goal is to better assist people in developing economies in reducing the health impacts of severe heat stress,” Guo added.
This pioneering research underscores the importance of considering humidity in models that predict the health impacts of climate change. By incorporating this often-overlooked factor, researchers and policymakers can better protect vulnerable populations from the increasing dangers posed by climate change.
Journal Reference:
Qiang Guo, Malcolm N. Mistry, Antonio Gasparrini, Masahiro Hashizume, Taikan Oki et al. ‘Regional variation in the role of humidity on city-level heat-related mortality’, PNAS Nexus (vol. 3, Iss. 8; 2024). DOI: 10.1093/pnasnexus/pgae290
Article Source:
Press Release/Material by University of Tokyo
Featured image credit: Freepik